Several years ago, I sat in a waiting room clutching my blue inhaler, blissfully unaware that this small rescue device carried a carbon load heavier than my morning drive to work. The more I dug into the numbers, the more my jaw dropped — one salbutamol inhaler can leave a footprint equivalent to driving over 290 kilometers. That realization sparked my obsession: how can something so life-giving have such an outsize cost, and what can we do about it?
Metered Dose Inhalers: A Life-Saver with a Carbon Shadow
My first memory of asthma relief is vivid: the reassuring click and cool mist of my blue metered dose inhaler (pMDI). Like millions worldwide, I relied on this small device to breathe easy. What I didn’t realize then was that this life-saver carried a hidden environmental cost. “I had no idea my inhaler emissions could stack up like a year’s worth of road trips.”
How Metered Dose Inhalers Work—and Why They Matter
Metered dose inhalers are the gold standard for emergency asthma and COPD treatment. They deliver a precise dose of medicine deep into the lungs, thanks to hydrofluoroalkane (HFA) propellants. These HFA propellants—like HFA-134a and HFA-227ea—are what give pMDIs their “punch,” propelling medication quickly and effectively.
But here’s the catch: these same HFA propellants are potent greenhouse gases. They trap heat thousands of times more effectively than carbon dioxide (CO₂). In fact, each gram of HFA-134a has the same global warming potential (GWP) as 1.4 kilograms of CO₂, while HFA-227ea is even higher.
The Hidden Environmental Impact: Each Inhaler Like a Mini Road Trip
It’s easy to overlook the environmental impact of something so small. But the numbers are startling. A single typical pMDI, containing 200 doses, is responsible for about 28 kg CO₂ equivalent—roughly the same as driving a car for 300 kilometers. That means every time I used my inhaler, I was unwittingly adding to my carbon footprint in a big way.
Globally, the scale is even more dramatic. In 2019, over 480 million pMDI packs were prescribed—dispensing 2,400 doses every second worldwide. In the United States alone, HFA MDI use in 2020 generated 2.5 million metric tons of CO₂ equivalent, which is comparable to the annual emissions from 550,000 cars.
Where the Emissions Come From: The Surprising Twist
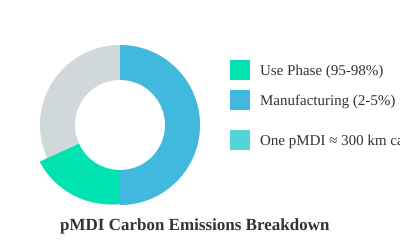
One of the most surprising facts I discovered is that almost all of a pMDI’s carbon footprint comes from its use, not its manufacture. 95–98% of emissions are released when the inhaler is used and the propellant escapes into the atmosphere. Manufacturing and packaging account for only 2–5%.
‘I had no idea my inhaler emissions could stack up like a year’s worth of road trips.’
Global Scale and Healthcare’s Carbon Burden
- pMDIs account for 3–4% of the UK NHS’s carbon footprint.
- At GSK, MDIs are responsible for 45% of total corporate emissions.
- Inhaler use patterns vary: 88% of US inhalers are pMDIs, compared to just 13% in Sweden.
- Worldwide, pMDIs contribute about 0.03% of total global greenhouse gas emissions.
Visualizing the Carbon Shadow
Metered dose inhalers are essential for millions, but their environmental impact is far from negligible. With each puff, we’re not just breathing easier—we’re also adding to a global carbon shadow that’s finally coming into focus.
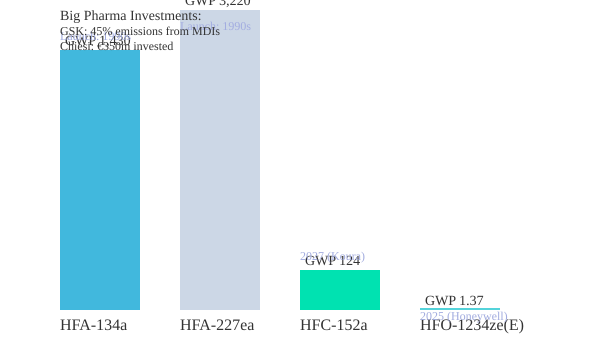
The Propellant Dilemma: Big Pharma’s Race to Go Green
As I dig into the environmental impact of inhalers, it’s clear that the real issue lies in the propellants used in most metered dose inhalers (MDIs). These are typically hydrofluoroalkane (HFA) propellants, which have shockingly high Global Warming Potential (GWP). For context, HFA-134a has a GWP of 1,430, and HFA-227ea is even higher at 3,220—meaning each gram released is as damaging as 1.4 to 3.2 kilograms of CO₂ over a century. With hundreds of millions of inhalers prescribed each year, the cumulative effect is massive. In 2020, U.S. emissions from HFA MDIs alone reached 2.5 million metric tons of CO₂ equivalent—comparable to the annual emissions of over half a million cars.
Why Are HFA Propellants So Potent?
HFAs were introduced as a safer alternative to ozone-depleting CFCs, but their chemical structure makes them powerful greenhouse gases. They linger in the atmosphere, trapping heat far more effectively than CO₂. In healthcare, inhaler propellants are among the highest GWP substances still in regular use.
Industry’s Green Response: Big Pharma Steps Up
Recognizing both the environmental and regulatory pressures, the pharmaceutical industry is racing to develop greener alternatives. Giants like GSK and AstraZeneca are investing heavily in sustainable inhaler manufacturing and next-generation propellants. As one internal company source put it:
“Making our inhalers cleaner could be one of the fastest wins for pharma’s climate footprint.”
GSK reports that MDIs account for 45% of its total corporate emissions, prompting a major push to reformulate products like Ventolin for a 90% smaller climate impact. Chiesi has committed €350 million to green inhaler development and recycling, while AstraZeneca is transitioning its Breztri inhaler to new low-GWP propellants.
The New Wave: Ultra-Low-GWP Propellants
- HFC-152a (Zephex® 152a): With a GWP of 124—90% lower than HFA-134a—this propellant is set for commercial supply by 2027 (Koura). It offers a dramatic reduction in climate impact while maintaining inhaler performance.
- HFO-1234ze(E) (Solstice® Air): This propellant stands out with a GWP of just 1.37, a 99.9% reduction compared to HFA-134a. Honeywell expects commercial launch as early as 2025, and clinical trials show it works just as well for patients.
Kigali Amendment Impact and Regulatory Squeeze
International agreements like the Kigali Amendment to the Montreal Protocol, along with EU and US regulations, are making high-GWP HFAs increasingly expensive—propellant costs could rise up to five-fold by 2025. This regulatory push is accelerating the shift to greener technologies and making sustainable inhaler manufacturing a top industry priority.
Sustainable Production: Beyond the Propellant
Pharma’s green race isn’t just about new propellants. Companies are also investing in energy-efficient manufacturing, recycled materials, and circular economy initiatives. Chiesi’s Take AIR program, for example, focuses on recycling inhalers and recovering used propellants safely. These steps are essential for reducing the overall carbon footprint of inhaler products.
The Rise of Green Inhalers: Patient Experience & Practical Barriers
When my father turned 70, his doctor suggested switching from his familiar metered dose inhaler (pMDI) to a dry powder inhaler (DPI). As someone passionate about both respiratory health and sustainability, I volunteered to help him learn the new device. At first, he was hesitant—worried about change and whether it would work as well. But after a few weeks, he was surprised at how simple the DPI was to use, and even more pleased to learn that it had a fraction of the environmental impact.
Dry Powder Inhalers & Soft Mist Inhalers: Lower Carbon, High Satisfaction
DPIs and soft mist inhalers (SMIs) are at the heart of the green inhaler revolution. Unlike pMDIs, which rely on high global warming potential (GWP) propellants, DPIs and SMIs are propellant-free. The numbers are striking: each DPI typically produces just 1–2 kg CO₂ equivalent (CO₂e) per device, compared to 28 kg for a standard pMDI. SMIs, especially reusable models, go even further—down to 0.78 kg CO₂e per device, with reusable options cutting emissions by up to 71% more.
But do these greener inhalers work as well? Clinical evidence says yes. Randomized trials and real-world studies consistently show that, when used correctly, DPIs and SMIs match or even outperform pMDIs in asthma control. For example, a large Lebanese study found that correct administration technique was achieved by 67.8% of DPI users, compared to just 38.4% for pMDIs. Exacerbation rates were also lower: 21.7% for DPIs versus 59.4% for pMDIs.
Patient Preferences: Satisfaction and Environmental Awareness
Patient experience is a key part of the story. After making the switch, over 74% of new DPI users rated their inhaler as “very good” after just 12 weeks, compared to only 13.4% for their previous pMDI. As one patient put it:
“After my switch, breathing easier meant shrinking my carbon shadow, too.”
Environmental concerns are increasingly influencing choices. Surveys show that patients rate the carbon footprint of their inhaler as 3.4 out of 5 in importance, and most are willing to change devices to reduce their impact. The NHS Low-GWP Inhaler initiative and similar programs are helping to embed sustainability into routine care.
Who Can—and Can’t—Switch?
While many patients can benefit from DPIs and SMIs, thoughtful device selection is crucial:
- Very young children and elderly patients with weak inhalation may struggle to generate enough inspiratory flow for DPIs.
- People with milk protein allergies cannot use lactose-based DPIs.
- During acute asthma attacks, pMDIs may still be preferred for rapid relief.
However, with proper patient counseling and training, most adults can transition successfully. In the U.S. Veterans Association health system, 74.9% of over 347,000 patients completed a switch from pMDI to DPI, with only 14.2% returning to their original device.
Education, Training, and Support: The Key to Success
Change isn’t always smooth, but it’s rewarding. Education and support are essential for successful, equitable transitions. Decision aids—like those from NICE—and structured patient counseling help match the right device to the right person. Programs such as Chiesi’s Take AIR also support sustainability through inhaler recycling and safe propellant recovery.
Ultimately, the rise of green inhalers shows that with the right support, patients can breathe easier—while shrinking their carbon shadow.
What’s Next? Inventing the Future of Sustainable Respiratory Care
As I reflect on the urgent environmental challenge posed by traditional inhalers, it’s clear that we’re standing at the edge of a green revolution—one puff at a time. The shift toward sustainable inhaler manufacturing is not just a technical upgrade; it’s a fundamental reimagining of how respiratory care can help drive healthcare system decarbonization worldwide. With every innovation, we move closer to a future where breathing easy doesn’t come at the planet’s expense.
Imagine a world where inhalers are part of a true circular economy: manufactured using renewable energy, designed for full recyclability, and supported by robust take-back programs for safe propellant recovery. This isn’t a distant dream. Already, companies are investing in next-generation propellants like HFC-152a and HFO-1234ze(E), which slash the global warming potential of inhalers by more than 90%. Meanwhile, propellant-free devices like dry powder and soft mist inhalers are setting new standards for low-carbon respiratory care. If these green inhalers are adopted at scale, projections show a dramatic 85% drop in healthcare’s global warming potential by 2035, with inhaler-related emissions shrinking from about 20 million to less than 1 million tonnes of CO₂ equivalent each year.
But as we accelerate this transformation, I recognize that regulatory responses and international policy alignment are the wild cards. The rules that govern inhaler approval and distribution can either speed up or stall progress. Harmonizing standards across borders is crucial to ensure that patients everywhere have timely access to safe, effective, and environmentally friendly options. As one representative from the European Network on Climate and Health Education put it,
‘Decarbonizing healthcare isn’t just about science—it’s a collaboration between industry, providers, patients, and policymakers.’
Yet, there’s an equity warning we can’t ignore. Green technology must not leave low-resource patients or countries behind. The cost of new inhalers and the infrastructure needed for recycling or take-back programs could widen global health gaps if not addressed through technology transfer, capacity building, and strong international partnerships. Ensuring global equity and regulatory alignment is the last hurdle before we reach a net-zero horizon in respiratory care.
Education will be the bridge to success. Patients and providers alike need support to navigate device choices, master new techniques, and understand the environmental impact of their prescriptions. Healthcare systems like the NHS are leading the way, embedding sustainability into clinical guidelines and targeting net-zero emissions by 2040. These efforts show that healthcare emissions reduction is not only possible—it’s within reach.
In conclusion, the journey toward sustainable respiratory care is about more than just swapping out propellants. It’s about building a future where every breath supports both personal health and planetary well-being. With circular manufacturing, smart regulation, global equity, and shared commitment, we can invent a model for decarbonized, effective, and fair healthcare—one that truly lets us all breathe easy.
TL;DR: Metered dose inhalers, though vital for millions, have a surprisingly outsized environmental impact due to their propellant gases — but major innovations and patient-driven change are paving the way for much greener respiratory care.

Comments
Post a Comment